Patient engagement technology involves digital platforms and tools that facilitate active patient participation in healthcare decision-making, treatment adherence, and health management through secure communication channels, educational resources, and remote monitoring capabilities. These comprehensive solutions enable healthcare organizations to extend their reach beyond clinical settings while maintaining continuous connections with patients between appointments. Modern patient engagement technology integrates with electronic health records, practice management systems, and clinical workflows to create seamless experiences that improve health outcomes, reduce costs, and enhance patient satisfaction across diverse healthcare settings.
Digital Communication Platforms and Secure Messaging
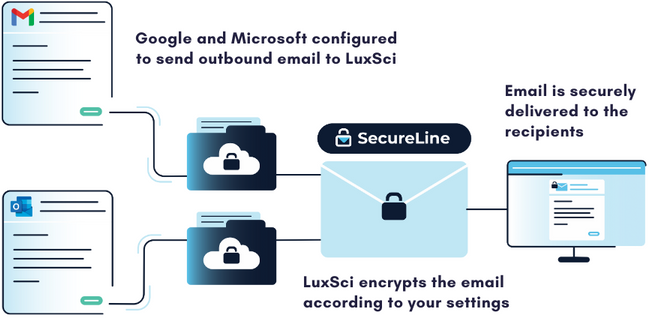
Secure messaging platforms enable real-time communication between patients and healthcare teams through encrypted channels that protect sensitive health information during transmission and storage. These communication tools allow patients to ask questions about their treatment plans, report symptom changes, and request prescription refills without requiring telephone calls during busy clinical hours. Healthcare providers can respond to patient inquiries efficiently while maintaining detailed documentation of all communications that integrate seamlessly with electronic health record systems.
Video consultation capabilities expand access to healthcare services by enabling remote consultations that eliminate geographic barriers and transportation challenges for patients. Telehealth integration within patient engagement technology provides scheduling, documentation, and billing support that streamlines virtual care delivery while maintaining the same security standards as in-person visits. Mobile applications extend communication opportunities by allowing patients to connect with their healthcare providers from smartphones and tablets, increasing engagement accessibility for diverse patient populations.
Patient portal functionality creates centralized hubs where individuals can access their complete health information, review test results, and communicate with multiple providers involved in their care coordination. These portals enable patients to download medical records, share information with family members or other healthcare providers, and maintain personal health records that support informed decision-making. Integration capabilities ensure that patient communications and data sharing activities are properly documented within clinical systems while maintaining appropriate privacy protections.
Automated communication systems deliver appointment reminders, medication alerts, and health education content through patients’ preferred communication channels including email, text messaging, and mobile push notifications. These automated touchpoints maintain patient engagement between visits while reducing no-show rates and improving medication adherence through timely reminders. Customization options allow healthcare organizations to tailor communication frequency and content based on individual patient preferences and clinical requirements.
Remote Monitoring and Health Data Collection
Wearable device integration enables continuous health monitoring that provides healthcare teams with real-time data about patient activity levels, vital signs, and symptom patterns between clinical encounters. Patient engagement technology platforms can collect data from fitness trackers, blood pressure monitors, glucose meters, and other connected devices to create comprehensive pictures of patient health status. This continuous monitoring capability allows healthcare providers to identify concerning trends early and intervene before conditions require emergency treatment or hospitalization.
Home monitoring systems enable patients with chronic conditions to track their health metrics daily and share this information automatically with their healthcare teams through secure data transmission protocols. Heart failure patients can monitor their weight and symptoms through connected scales and symptom tracking applications that alert providers when concerning changes occur. Diabetic patients can share glucose readings, medication compliance data, and lifestyle factors that help providers optimize treatment plans based on real-world behavior patterns rather than periodic clinic visit snapshots.
Patient-reported outcomes collection through digital surveys and questionnaires provides healthcare teams with structured data about symptom severity, treatment effectiveness, and quality of life impacts that support clinical decision-making. These digital assessment tools can be deployed before appointments to help patients prepare for visits and enable providers to focus consultation time on addressing specific concerns rather than gathering basic information. Longitudinal tracking of patient-reported outcomes helps healthcare teams measure treatment effectiveness over time and adjust care plans based on patient experiences.
Data visualization tools transform complex health information into understandable charts and graphs that help patients comprehend their health trends and treatment progress. Interactive dashboards enable patients to explore their health data, set personal goals, and track their progress toward achieving better health outcomes. These visualization capabilities empower patients to take active roles in their healthcare management by providing clear feedback about how their behaviors and treatment adherence affect their health status.
Educational Resources and Health Literacy Support
Personalized health education delivery through patient engagement technology ensures that individuals receive relevant information about their specific conditions, treatment options, and prevention strategies. Content management systems enable healthcare organizations to create libraries of educational materials that can be customized based on patient diagnoses, treatment plans, and health literacy levels. Multilingual content support accommodates diverse patient populations while interactive formats improve information retention compared to static printed materials.
Video education libraries provide patients with visual learning opportunities that demonstrate proper medication administration, exercise techniques, and self-care procedures that support treatment plan adherence. Professional-quality educational videos can be integrated into patient portals and mobile applications to provide convenient access to learning resources whenever patients need information or reminders. Progress tracking capabilities enable healthcare providers to monitor which educational materials patients have accessed and identify knowledge gaps that may require additional support.
Interactive decision support tools help patients understand treatment options, potential risks and benefits, and expected outcomes to support informed consent and shared decision-making processes. These digital tools can present complex medical information in accessible formats that help patients evaluate their preferences and values when choosing between different treatment approaches. Decision aids have been shown to improve patient satisfaction with treatment choices and reduce decision regret by ensuring patients understand their options thoroughly.
Health coaching platforms provide structured support programs that guide patients through behavior change processes using evidence-based techniques and motivational strategies. Digital coaching tools can deliver personalized goal-setting assistance, progress tracking, and encouragement messages that help patients develop healthy habits and maintain treatment adherence over time. Integration with clinical workflows enables healthcare providers to monitor patient coaching program participation and adjust clinical support based on patient engagement levels and progress toward health goals.
Care Coordination and Team Communication
Multi-provider communication tools enable seamless information sharing between primary care physicians, specialists, and other healthcare team members involved in patient care coordination. Patient engagement technology can facilitate secure messaging between providers, appointment scheduling coordination, and treatment plan sharing that ensures all team members have access to current patient information. Care team directories help patients understand their healthcare team composition and know whom to contact for different types of questions or concerns.
Care plan management systems create structured frameworks for coordinating complex treatment regimens that involve multiple providers, medications, and lifestyle modifications. Digital care plans can be shared with patients and all members of their healthcare team to ensure everyone understands treatment goals, responsibilities, and timelines for achieving desired outcomes. Progress tracking capabilities enable care teams to monitor patient adherence to treatment plans and identify areas where additional support may be needed.
Referral management tools streamline the process of connecting patients with specialist care by enabling electronic referral submission, appointment scheduling coordination, and information sharing between referring and receiving providers. Patient engagement technology can automate referral status updates, provide patients with clear instructions for specialist visits, and ensure that all relevant medical information is available to consulting physicians. These coordination tools reduce delays in specialty care access while improving communication between all parties involved in referral processes.
Family member access controls enable patients to grant appropriate family members or caregivers access to their health information and communication platforms while maintaining privacy boundaries they feel comfortable with. Caregiver portal functionality allows family members to help manage appointments, medication reminders, and communication with healthcare providers when patients need assistance with technology or health management tasks. These collaborative features support patients who may have cognitive impairments, mobility limitations, or other challenges that make independent health management difficult.
Clinical Workflow Integration and Provider Tools
Electronic health record integration ensures that all patient engagement activities are properly documented within clinical systems and available to providers during patient encounters. API connectivity enables patient communications, health monitoring data, and engagement metrics to populate appropriate sections of medical records automatically. Real-time data synchronization ensures that providers have access to the most current patient information when making clinical decisions or responding to patient inquiries.
Clinical decision support integration provides healthcare teams with alerts and recommendations based on patient engagement data and health monitoring information. These tools can identify patients who may be experiencing medication adherence problems, concerning symptom changes, or gaps in preventive care based on their engagement patterns and reported information. Automated alerts enable proactive intervention before problems escalate to require emergency care or hospitalization.
Provider dashboard tools aggregate patient engagement metrics, communication volumes, and health monitoring data to help healthcare teams manage their patient populations efficiently. These dashboards can identify patients who may need additional support, highlight concerning health trends across patient populations, and provide insights into engagement program effectiveness. Analytics capabilities enable healthcare organizations to measure the impact of patient engagement technology on clinical outcomes, patient satisfaction, and operational efficiency.
Workflow automation tools reduce administrative burden on healthcare staff by automating routine tasks like appointment confirmations, medication refill approvals, and routine health screening reminders. These automation capabilities free up staff time for higher-value activities like patient education, care coordination, and complex problem-solving. Customizable automation rules enable healthcare organizations to tailor workflow support to their specific operational requirements and patient population needs.
Implementation Strategies and Change Management
Phased deployment approaches enable healthcare organizations to implement patient engagement technology gradually while managing change effectively and minimizing workflow disruption. Organizations might begin with basic secure messaging functionality before expanding to include remote monitoring, educational resources, and advanced care coordination tools. This incremental approach allows staff and patients to adapt to new technologies progressively while enabling organizations to address challenges and optimize workflows before full-scale deployment.
Staff training programs prepare healthcare teams to use patient engagement technology effectively while maintaining productivity and patient care quality during implementation periods. Training should address both technology usage and workflow changes that result from implementing digital patient engagement tools. Change management strategies help overcome resistance to new technologies while ensuring consistent adoption across all departments and provider types within healthcare organizations.
Patient onboarding procedures ensure that individuals understand how to access and use engagement technology platforms while maintaining security standards and protecting their health information. Training materials should accommodate different technology comfort levels and provide multiple learning formats including written instructions, video tutorials, and in-person assistance. Support resources should be readily available to help patients troubleshoot problems and maximize their engagement with available tools and resources.
Success measurement frameworks enable healthcare organizations to evaluate the effectiveness of patient engagement technology investments through objective metrics and patient feedback. Key performance indicators might include engagement rates, patient satisfaction scores, clinical outcome improvements, and operational efficiency gains. Regular assessment procedures help organizations optimize their technology deployments and demonstrate return on investment to stakeholders and leadership teams.