A HIPAA compliant form refers to any document or electronic form used to collect, access, or store protected health information (PHI), while also meeting the privacy and security requirements outlined by the Health Insurance Portability and Accountability Act (HIPAA). In healthcare today, patient data is one of the most valuable assets that any provider, payer or supplier can possess. As well as being highly valuable, however, the nature of patient data also makes it highly sensitive. That’s where HIPAA compliant forms come in. HIPAA is designed to safeguard patient data and protect health information (PHI) from unauthorized access, disclosure, and use.
With the rise of digital interactions in the healthcare industry, one of the best ways to capture and manage sensitive data is through secure forms. Whether onboarding new patients, scheduling appointments, gathering patient feedback, conducting surveys, or carrying out marketing campaigns, securely collecting patient information and business intelligence via HIPAA compliant forms can provide huge opportunities for improved efficiency and a better overall patient or customer experience.
In this article, we’ll explore the essential role secure forms play in collecting patient data, why healthcare companies should use HIPAA compliant forms to capture PHI, and subsequently, how to create secure and compliant forms for use in your everyday healthcare operations.
Why HIPAA Compliant Forms are Crucial for Healthcare?
A secure form (or secure web form) is a type of online form designed to collect, transmit, and store data and business intelligence, while maintaining strict security standards, including compliance with HIPAA regulations. Secure forms typically incorporate encryption and authentication protocols to ensure data is protected from unauthorized access during submission and storage.
In the context of healthcare, secure forms are specifically designed to capture PHI, which includes a patient’s name, address, medical history, diagnoses, treatment plans and other personal details related to their health.
Healthcare organizations, such as hospitals, doctors’ offices, clinics, in-home care services, retail healthcare, testing services and laboratories, health plan administrators, insurers, and medical equipment providers all deal with patient data on a daily basis. The sensitive and important nature of this data makes it a prime target for cybercriminals, who seek to use it for financial gain or other malicious purposes, including disrupting critical infrastructure and business operations, identity theft, and more.
Accounting for this, when scheduling appointments, onboarding new patients, or conducting surveys, for example, healthcare companies must use secure forms that adhere to HIPAA guidelines to ensure patient data is properly secured.
These include:
- Data is encrypted in transit, when being collected from the form and transferred to storage, and at rest, where the patient data will reside, i.e. in a database.
- Only authorized users, i.e., employees with good reason to handle PHI, have access to patient data.
- Authorized users are also properly authenticated, to ensure they are who they claim to be, i.e., credentials haven’t been stolen, a session hasn’t been hijacked, etc.
Conversely, using unsecured forms to collect PHI could result in the data being compromised in a breach—and your organization suffering the associated consequences. As well as the financial penalties of a security breach, such as fines and compensation paid to the affected parties, more significantly, you’ll incur a dent in your reputation of your business and a loss of patient trust.
Key Applications for Secure Forms in Healthcare
Now that we’ve covered why HIPAA compliant forms are vital for healthcare organizations, let’s look at some of the most effective ways they can be utilized.
1. New Patient Onboarding and Registration
Gathering basic information, such as their medical history, insurance details, and personal information, is a fundamental part of onboarding new patients. Secure forms allow patients to submit their sensitive data through a safe, encrypted platform, mitigating the risk of data exposure considerably and reducing or eliminating the need for human intervention in the process.
Additionally, automated form submissions, using data from electronic health record (EHR) systems and other integrated tools save time for healthcare providers and patients, offering a streamlined registration experience and improved workflows.
2. Appointment Scheduling
Secure forms offer an efficient way for patients to schedule their appointments, reducing time, effort, and administrative overhead by eliminating the need for a phone call or back-and-forth email conversation through automated scheduling. When integrated properly, the completion of a secure form can trigger appointment confirmation and reminder emails to reduce missed appointments. Allowing patients to book appointments in this way drastically reduces the amount of friction involved, making it far easier for patients to comply and making sure they don’t miss appointments.
3. Patient and Customer Surveys
Feedback from patients plays a crucial role in improving healthcare services and experiences, allowing companies to pinpoint areas for refinement. Requesting feedback is also highly beneficial for a company’s long-term relationship with a patient or customers, as it demonstrates they value their opinion and want to incorporate it into their ongoing commitment to excellent service and efficient healthcare journeys; this makes patients more inclined to trust them, strengthening their connection and overall engagement.
Whether for patient satisfaction surveys or follow-up care assessments, secure forms offer a compliant means of collecting valuable feedback without jeopardizing PHI.
4. Email Communications and Marketing Campaigns
Email marketing in healthcare can be a tricky endeavor, especially when it comes to getting patients to opt-in and for classifying and handling PHI.
By using secure forms, healthcare organizations can gather consent from patients for email communications and marketing campaigns. Secure forms ensure that any sensitive patient data (i.e., preferences for specific treatments or communications) is submitted safely and stored in compliance with privacy regulations.
End-to-End Security for Form Data
An essential requirement of secure forms used by healthcare providers, payers, and suppliers is that they provide end-to-end security, i.e., protecting form data throughout its entire lifecycle—from submission to storage to access. Here are the measures required to ensure end-to-end security for PHI captured by web forms.
1. Secure Transmission
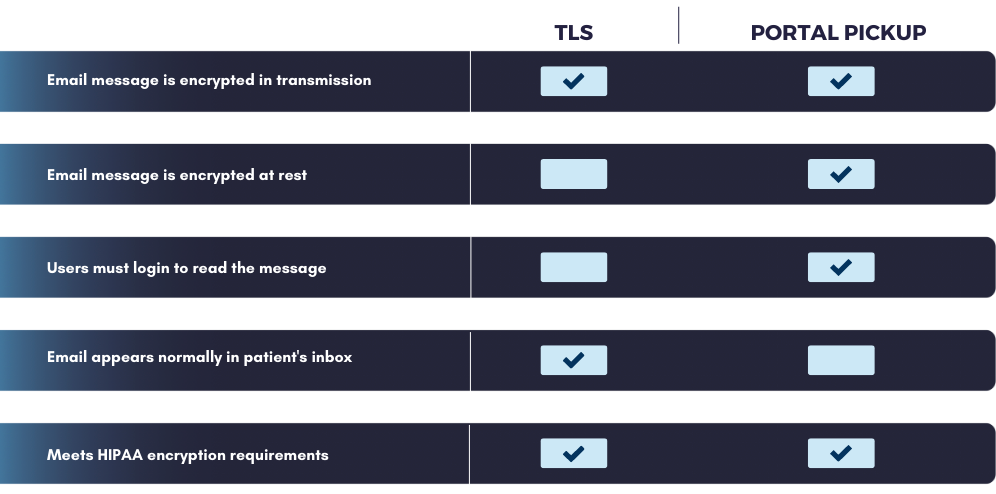
As alluded to earlier, when a patient submits data through a form, it must be encrypted while being transmitted from the form, i.e., the place of capture, to where it will be stored. Using Secure Socket Layer (SSL) or Transport Layer Security (TLS) encryption ensures that sensitive data, such as PHI, is protected from interception by malicious actors.
2. Secure Storage
Similarly, after submission, form data must be stored securely in an encrypted database to ensure HIPAA compliance. Subsequently, in the event the database is breached and the PHI exfiltrated, it will be undecipherable to cybercriminals, protecting the data from exposure.
3. Access Control and User Authentication
Organizations must ensure that only authorized personnel can access sensitive patient data, according to their responsibilities regarding PHI. In addition to this, healthcare organizations must implement strong authentication mechanisms, such as multi-factor authentication (MFA) and robust password practices, to facilitate user authentication. These mitigation measures are interconnected as they help better secure data even if a hacker gets their hands on an authorized employee’s login details.
4. Audit Logs
Additionally, companies must maintain audit, or activity, logs to carefully track who accessed PHI, when, where they accessed it from, and why, i.e., how they acted upon the data. This helps identify suspicious or malicious behavior and, in the event of a breach, pinpoint its origin and contain its spread. Audit logs can also reveal which employees have too many access privileges, enabling healthcare organizations to tighten up their access control policies.
Best Practices for Secure Forms
Finally, here are some best practices to align with when employing the use of secure forms to collect patient data.
1. Use a Secure Form Builder
Choose a solution, such as LuxSci, that specializes in secure, HIPAA compliant forms. This ensures that all data collection, transmission, and storage are adequately encrypted and that compliance standards are met.
2. Enable Encryption
Always use encryption protocols, such as SSL or TLS, to protect data in transit, as well as encrypted databases, to store data. This ensures that data, especially sensitive PHI, remains encrypted according to HIPAA regulations.
3. Implement Role-Based Access
Ensure that access to sensitive data collected from forms is restricted based on roles within your organization. Only those who need the data to perform their jobs should have access, i.e., role-based access control (RBAC).
4. Keep Forms Simple
Avoid overwhelming patients and customers with too many fields or questions and focus on collecting the essential data necessary for the task at hand. This increases the likelihood the form will be filled out correctly and you’ll capture all necessary PHI.
5. Test Your Forms
Regularly test your forms for user experience, security vulnerabilities and functionality issues. Vulnerabilities in your forms could lead to data breaches or compliance violations, so regularly probing your forms for weaknesses, and acquiring up-to-date data intelligence to discover emerging threats, ensures they remain secure.
Why LuxSci’s Secure Forms Stand Out
LuxSci offers a fully HIPAA compliant Secure Forms solution, designed specifically with the security needs of healthcare organizations in mind. This includes:
- End-to-End Security: Data is protected through advanced encryption protocols during transmission and storage, ensuring patient data remains confidential.
- Customization: Forms can be easily created and customized to collect a wide range of patient and customer information, including PHI, appointment details, feedback, and consent for communications.
- Seamless Integration: The LuxSci Secure Forms solution integrates with existing healthcare systems that store PHI to enable streamlined workflows and centralized data management.
- Audit Trails: LuxSci provides comprehensive audit logging to track every action taken on the data, offering accountability and transparency in accordance with HIPPA guidelines.
Want to learn more about how LuxSci’s Secure Forms will help you achieve HIPAA-compliant patient data collection? Contact us today to talk with our expert team.
HIPAA Compliant Forms FAQs
1. What is the difference between a secure form and a regular form?
A secure form uses encryption and security protocols to ensure that data is protected during transmission and storage. Regular forms don’t necessarily offer these risk mitigation measures, making them far more vulnerable to data breaches, especially in healthcare.
2. Is LuxSci’s Secure Forms solution HIPAA-compliant?
Yes, LuxSci’s Secure Forms are fully HIPAA-compliant, ensuring the privacy and security of Protected Health Information (PHI).
3. How does encryption work in secure forms?
Encryption transforms data into unreadable code during transmission and at rest, so only authorized recipients with the decryption key can access the original data, ensuring that sensitive information remains confidential—even in the event of a breach.
4. Can secure forms be integrated with other healthcare systems?
Yes, LuxSci Secure Forms integrate seamlessly with other healthcare systems, platforms and applications, including customer data platforms (CDPs), electronic health records (EHR) systems, and revenue cycle management (RCM) platforms, making it easier to manage collected data—and, better still, keep it secured.
5. Why is end-to-end security important for healthcare forms?
End-to-end security ensures that patient data remains protected throughout the entire process—from submission to storage to subsequent access. This reduces the risk of data breaches and ensures HIPAA compliance.