Ensuring HIPAA compliance for email is crucial for healthcare organizations and their business associates when handling Protected Health Information (PHI). HIPAA regulations require strict safeguards, including access controls, audit logs, integrity protections, and transmission security, to prevent unauthorized access and breaches. Encryption plays a key role in securing PHI during email exchanges, and organizations must establish comprehensive email policies aligned with the HIPAA Privacy Rule. Additionally, some state laws may impose stricter requirements, such as obtaining explicit patient consent before using email for PHI. Understanding these regulations is essential for maintaining compliance, protecting patient data, and avoiding costly penalties.
The Health Insurance Portability and Accountability Act (HIPAA) is a complicated law that sets the standards for collecting, transmitting, and storing protected health information (PHI). When information is stored or exchanged electronically, the HIPAA Security and Privacy Rules require covered entities to safeguard its integrity and confidentiality. One of the most common ways that PHI is shared electronically is via email. Understanding how HIPAA email rules apply is essential to meet HIPAA requirements and protect sensitive data.
The HIPAA Email Security Rule
It’s important to note that HIPAA does not require the use of any specific technology or vendor to meet its requirements. Generally speaking, the Security Rule requirements for email fall into four categories:
- Organizational requirements state the specific functions a covered entity must perform, including implementing policies and procedures and obligations concerning business associate contracts.
- Administrative requirements relate to employee training, professional development, and management of PHI.
- Physical safeguards encompass the security of computer systems, servers, and networks, access to the facility and workstations, data backup and storage, and the destruction of obsolete data.
- Technical safeguards ensure the security of email data transmitted over an open electronic network and the storage of that data.
Below, we discuss some of the main requirements that apply to email and the steps you need to take to secure email accounts that transmit and store PHI.

HIPAA Compliance Email Rules
While email encryption gets most of the spotlight during discussions on HIPAA compliant email security, HIPAA regulations for email cover a range of behaviors, controls, and services that work together to address eight key areas.
1. Access: Access controls help safeguard access to your email accounts and messages. Implementing access controls is essential to keep out unauthorized users and secure your data. Some key steps to take include:
- Using strong passwords that cannot be easily guessed or memorized.
- Creating different passwords for different sites and applications.
- Using two-factor authentication.
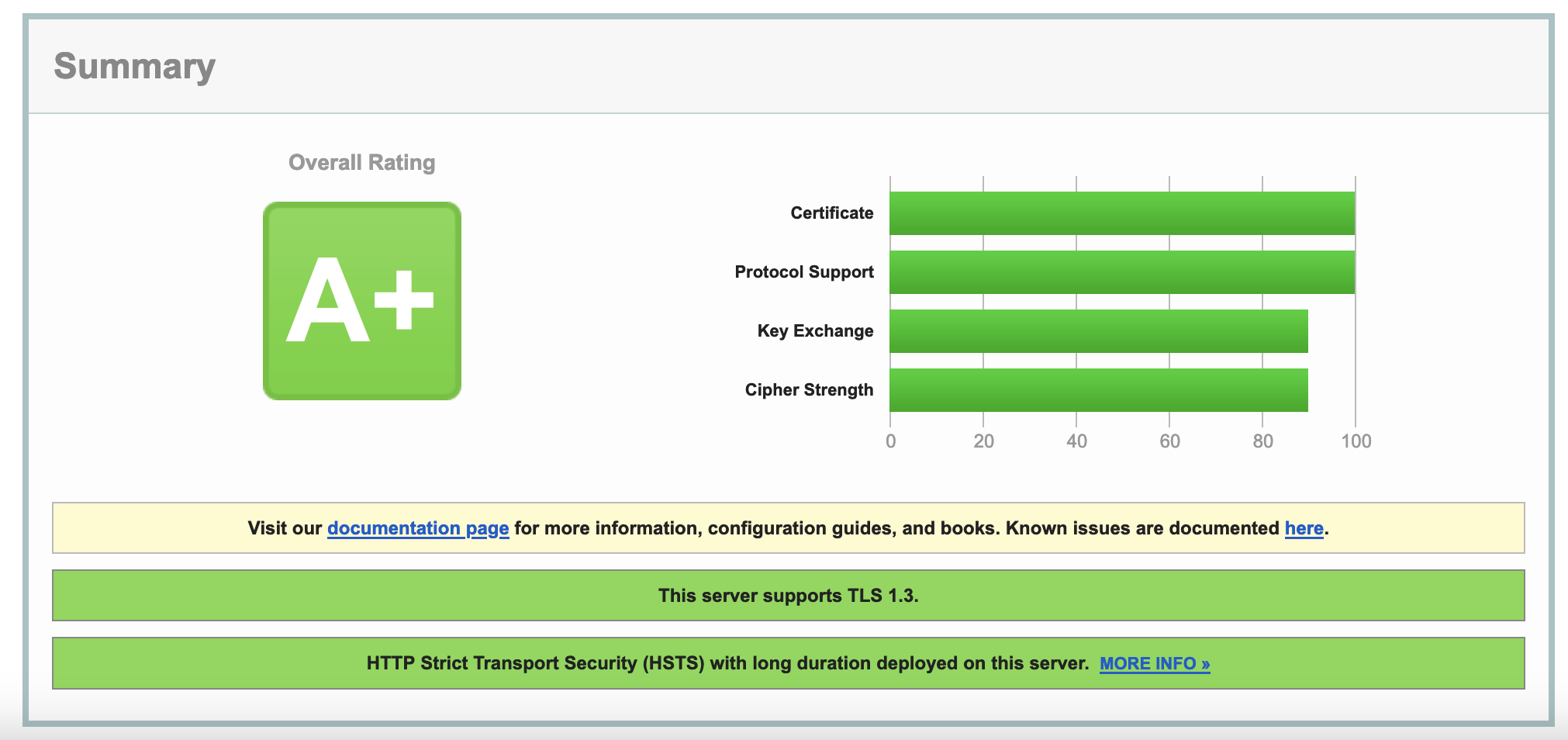
- Securing connections to your email service provider using TLS and a VPN.
- Blocking unencrypted connections.
- Being prepared with software that remotely wipes sensitive email off your mobile device when it is stolen or misplaced.
- Logging off from your system when it is not in use and when employees are away from workstations.
- Emphasizing opt-out email encryption to minimize breaches resulting from human error.
2. Encryption: Email is inherently insecure and at risk of being read, stolen, eavesdropped on, modified, and forged (repudiated). Covered entities should go beyond the technical safeguards of the HIPAA Security Rule and take steps beyond what is required to futureproof their communications. Some email encryption features to adopt include the following:
- The ability to send secure messages to anyone with any email address.
- The ability to receive secure messages from anyone.
- Implementing measures to prevent the insecure transmission of sensitive data via email.
- Exploring message retraction features to retrieve email messages sent to the wrong address.
- Avoiding opt-in encryption to satisfy HIPAA Omnibus Rule.
3. Backups and Archival: HIPAA email retention rules require copies of messages containing PHI to be retained for at least six years. To address these requirements, organizations must consider the following:
- How are email folders backed up?
- Are there at least two different backups at two different geographical locations? The processes updating these backups should be independent of each other as a measure against backup system failures.
- Have you maintained separate, permanent, and searchable archives? While the emails should be tamper-proof, with no way to delete or edit them, they should be easily retrievable to facilitate discovery, comply with audit requests, and support business-critical scenarios.
4. Defense: Cyber threats against healthcare organizations are continually increasing. Some may be surprised to learn that HIPAA secure email requirements mandate that organizations take steps to defend against possible attackers. To defend against malicious messages, consider implementing the following technologies:
- Server-side inbound email malware and anti-virus scanning to detect phishing and malicious links
- Showing the sender’s email address by default on received messages
- Email filtering software to detect fraudulent messages and ensure it uses SPF, DKIM, and DMARC information to classify messages
- Scanning outbound email
- Scanning workstations for malware and virus
- Using plain text previews of your messages
5. Authorization: A crucial aspect of HIPAA secure email requirements is ensuring that bad actors cannot impersonate your company or employees. Configuring your domains with SPF and DKIM is essential to verify your identity as an authorized sender of mail from your domains. Also, ensure that users cannot send messages through your email servers without authentication and encryption.
6. Reporting: Setting accountability standards for email security is essential to establishing and improving your HIPAA compliance posture. Some important steps to take include:
- Creating login audit trails.
- Receiving login failure and success alerts.
- Auto-blocking known attackers.
- Maintaining a log of all sent messages.
7. Reviews and Policies: Humans are the greatest vulnerability to any security and compliance plan. Create policies and procedures that focus on plugging vulnerabilities and preventing human errors. Some ways to reduce risk include:
- Inviting independent third parties to review your email policies and user settings. Fresh, unbiased eyes can weed out issues quickly.
- Disallowing the use of public Wi-Fi for devices that connect to your sensitive email.
- Creating email policies prohibiting users from clicking on links or opening attachments that are not expected or requested.
8. Vendor Management: Most people do not manage their email in-house. Properly vetting and researching whoever will be responsible for your email services is essential. Perform a yearly review of your email security and stay on top of emerging cybersecurity threats to take proactive action when necessary for sustained HIPAA compliance.
LuxSci’s secure email solutions were designed to help organizations tackle complicated HIPAA email rules. Contact us today to learn more how we can help you secure sensitive data.
Documenting HIPAA Compliance For Email
HIPAA compliant email requires documented proof that privacy and security protocols are being followed. HIPAA email systems must include audit trails, policy records, and incident response documentation that demonstrate appropriate safeguards are in place. Healthcare organizations benefit from clear documentation practices that satisfy regulatory inspectors while supporting daily operations and staff training activities.
Email Policy Documentation and Implementation Records
Healthcare organizations must develop written policies that govern HIPAA email usage according to Privacy Rule and Security Rule standards. Email policies should specify encryption requirements, staff responsibilities for handling patient information, and procedures for responding to security incidents. Policy documents must include implementation dates, responsible staff members, and update procedures when regulations change or organizational needs evolve.
Training records provide evidence that employees understand their HIPAA email obligations and can properly implement security procedures. Documentation should capture completion dates, training topics, assessment scores, and remedial training when staff members fail initial evaluations. Organizations that cannot produce training records struggle to prove employees received instruction appropriate to their job functions and access to patient information.
Business Associate Agreement files cover relationships with email service providers and other vendors handling protected health information. Contract documentation should include security specifications, incident reporting procedures, and audit rights that allow healthcare organizations to verify vendor performance. Without proper agreements, healthcare organizations expose themselves to liability when vendors mishandle patient information.
Risk assessment documentation identifies vulnerabilities in HIPAA email systems and describes corrective measures implemented to address identified problems. Assessment records should include evaluation methods, discovered issues, remediation plans, and verification that fixes have been properly implemented. Many organizations conduct risk assessments but fail to document their findings, making it difficult to track improvements over time.
Audit Trail Management and Log Analysis
HIPAA compliance for email depends on audit logs that track user activities, system access, and message handling throughout email platforms. Audit systems should capture login events, message transmission records, administrative changes, and security alerts that might indicate potential violations. Log protection prevents tampering while ensuring data remains accessible for regulatory review periods.
Monitoring systems can identify unusual email usage patterns that suggest security incidents or policy violations. Alert capabilities should flag failed login attempts, large file transfers, abnormal message volumes, and access from unauthorized locations. Real-time monitoring helps healthcare organizations respond quickly to potential security events before they escalate into breaches.
Log review schedules ensure audit data receives regular examination for potential security incidents or policy violations. Review procedures should specify analysis frequency, responsible personnel, and escalation steps when suspicious activities are discovered. Some entities collect extensive audit data but never review it, missing opportunities to identify security problems early.
Log retention policies balance storage costs with regulatory requirements and potential legal discovery obligations. Retention schedules should consider HIPAA requirements alongside other applicable regulations that might demand longer storage periods.Log data must be destroyed properly when retention periods expire to prevent unauthorized access to historical communications.
Incident Response Documentation and Breach Investigation
HIPAA email incident response procedures must address security events and human errors that might compromise patient information. Response plans should include assessment procedures, containment steps, investigation protocols, and notification requirements for different incident types. Quick response often determines whether a minor security event becomes a reportable breach.
Breach investigation procedures help healthcare organizations determine whether email incidents constitute breaches of unsecured protected health information under HIPAA definitions. Investigation protocols should include evidence collection methods, impact assessments, timeline development, and documentation standards that support internal decisions and potential regulatory reporting. Complex incidents may require external legal and technical expertise.
Notification procedures vary based on incident severity and the type of information potentially compromised. Internal notification processes ensure appropriate personnel are informed about incidents and can participate in response activities. Patient notification requirements create legal obligations that organizations must fulfill within timeframes established by federal regulations.
Corrective action documentation describes measures implemented to prevent similar incidents and demonstrates organizational commitment to improving email security. Action plans should include root cause analysis, remediation steps, implementation timelines, and verification procedures that confirm corrective measures work as intended. Organizations that implement fixes without documenting them may repeat the same mistakes when staff turnover occurs.
Staff Training Documentation and Competency Records
HIPAA email training programs must address technical email operations and regulatory requirements for handling protected health information. Training materials should cover encryption procedures, access controls, incident reporting, and acceptable use policies for email communications. Role-based training ensures different staff groups receive instruction appropriate to their job functions and patient information access levels.
Competency verification procedures help healthcare organizations confirm staff members understand and can properly implement HIPAA email security measures. Verification methods may include written tests, practical demonstrations, and performance monitoring that evaluate staff compliance with email policies. Training programs without competency verification cannot prove that employees actually learned the required information.
Refresher training schedules ensure staff members stay current with evolving threats, policy updates, and new email system features. Training frequency should consider technology change rates, emerging security threats, and organizational policy modifications. Staff members who received training years ago may not remember procedures or may have developed bad habits that compromise security.
Training effectiveness measurement helps healthcare organizations evaluate whether HIPAA email training programs meet learning objectives. Measurement approaches may include before and after assessments, incident rate analysis, and feedback collection that provide insights into training quality. Organizations should adjust training content based on effectiveness data to ensure educational efforts support compliance goals.
System Configuration and Change Control Records
Email system configuration documentation provides detailed records of security settings, access controls, and integration setups that support HIPAA compliance for email. Configuration records should include baseline security settings, approved modifications, and verification procedures that confirm systems maintain appropriate security levels. System administrators need current configuration records to troubleshoot problems and maintain security standards.
Change management procedures ensure modifications to HIPAA email systems receive proper evaluation, testing, and documentation before implementation. Change processes should include security impact assessments, testing protocols, approval workflows, and rollback procedures that minimize risks to email security. Changes made without proper documentation and approval create security vulnerabilities that may not be discovered until a breach occurs.
Version control procedures help healthcare organizations track changes to email system configurations and maintain the ability to restore previous settings when problems occur. Version documentation should include change descriptions, implementation dates, responsible personnel, and verification that modifications function properly. Organizations need version control to understand how their systems evolved and to reverse changes that cause problems.
Patch management procedures ensure email systems receive security updates promptly while maintaining system stability and compliance. Patch processes should include vulnerability assessment, testing protocols, deployment schedules, and verification that updates install correctly. Delayed patching leaves systems vulnerable to known exploits that criminals actively target.
HIPAA Compliant Email Vendor Management and Contract Documentation
Email service provider relationships must include Business Associate Agreements that specify security requirements, compliance obligations, and incident reporting procedures. Contract documentation should cover data handling standards, audit rights, and termination procedures that protect healthcare organizations when vendor relationships end. Regular vendor performance reviews ensure service providers continue meeting contractual obligations.
Vendor compliance verification ensures email service providers maintain their obligations under Business Associate Agreements and healthcare security standards. Verification activities may include security certification reviews, audit report analysis, and compliance documentation that demonstrates ongoing adherence to healthcare privacy requirements. Healthcare organizations that trust vendors without verification may discover compliance failures only after incidents occur.
Service level agreement documentation defines performance expectations, availability targets, and response times for email services and security incidents. Agreement records should include uptime guarantees, incident response procedures, and remediation steps when service levels are not met. Performance tracking helps healthcare organizations evaluate vendor reliability and compliance with contractual commitments.
Vendor communication records document interactions about security updates, policy changes, and compliance requirements that affect email services. Communication logs should include update notifications, compliance discussions, and resolution of security concerns that arise during vendor relationships. Good communication records help resolve disputes and ensure both parties understand their obligations when changes occur.